Today marks a week home from the hospital, and I'm so glad to be back. As anticipated, there has been some degree of a learning curve with the TPN at home, and new medication regimens, but so far, nothing that hasn't been remedied. Having nutrition has made a huge difference in post-hospital recovery time. There are some hiccups with transitioning off student health insurance, but we are trying to do what we can to make it as smooth as possible (after some panic). My new home health nurse is great, and is willing to deal with my twenty million questions and insistence upon sterility. I was able to go into work for part of a day so I could avoid taking a medical leave. This was a big relief, and also reassurance that I am passionate about what I do. I am incredibly lucky that my supervisor is extremely patient and accommodating. Even though graduate school is on hold for now, I am confident that trying to work a day or two a week (despite the hellish commute) will help keep me stimulated intellectually. It also gives me an additional sense of purpose as I focus more on spending time doing the things that I want to do and with my family. My little brother, Cody, started middle school this week, and it was really cool to be home to hear about his day.
In terms of health updates, I did my first methotrexate injection on Sunday, which is the low dose chemotherapy as an immunosuppressant. I certainly felt the side effects like nausea and some dizziness, and overall feeling crummy for the rest of the day, which I hope will decrease over time. Nevertheless, it was nothing unbearable, and something that I will do weekly. I also had my next round of IVIG outpatient today, which was the treatment that seemed to have caused the reaction that hospitalized me at the end of July. Thankfully, the small reactions I had were controllable, and I'm back at home resting.
Follow ups with my primary care physician and nephrology earlier in the week were also both largely uneventful. We are working out the logistics of the TPN with my primary care, and the nephrologist just confirmed what we already knew, which was that the autoimmune process is affecting my kidneys, and thus my electrolytes. We hope that the methotrexate, IVIG, and possibly another immune-modulating agent (to attempt once things stabilize more) can maybe help slow things down. I have follow ups next week in San Diego with allergy/immunology and cardiology. I also am supposed to get my new wheelchair tomorrow, which I think will be helpful particularly for work and times that I'm out and about. Still no news on when and if my port swap will be occurring, but the PICC line is driving me nuts based on where they placed it. It's right by the crease of my elbow, so when I bend my arm, the tubing rubs on the inside of my arm. and it pulls on the skin. Although its annoying, I'm lucky that it is fully functional, and as I have said before, the technology and science to be able to receive these treatments in an outpatient setting.
In addition to the two day San Diego trip for follow ups, I am hoping to get away for one night over Labor Day weekend. Going away for any reason ends up becoming quite the orchestration, and often rather stressful, but I think a change of scenery even just for 24 hours is worth a shot.
Tomorrow marks my grandmother Shelley's birthday, who passed away in April. I think it will be tough for all of us, but I know how much she loved all of the family, and would want us to celebrate her. If I'm up to it, maybe I'll try to hunt down one of her favorite desserts, lemon meringue pie :)
I hope that things will continue to be relatively uneventful, but will continue to past updates as they come.
A blog by Arielle, a twenty two year old with MCAS (Mast Cell Activation Syndrome), Autoimmune Angioedema, POTS (Postural Orthostatic Tachycardia Syndrome), Sjogren's Syndrome, immune deficiency, osteoporosis, and EDS (Ehlers Danlos Syndrome). Thoughts, feelings, academic endeavors, daily adventures (and misadventures). Pitzer College Class of 2018 (Psychology/Sociology) ---- UCLA Extension Patient Advocacy Certificate Program Winter 2019 ------ Family Resource Coach
Thursday, August 23, 2018
Thursday, August 16, 2018
Escape Plan Initiated
Finally I get to report that I should be on my way home this evening! Thank you again for all of you who have reached out, come to visit, dropped a note, it means a lot to me!
We were able to lower the IV steroids a hair more last night without any major episodes, and most of today was spent going back and forth between the pharmacy, home health/nursing agency, regular outpatient pharmacy, and my outpatient team to orchestrate everything. My situation is far from typical in terms of complexity and discharge, but we all can agree that virtually living in the hospital is not a very solid quality of life, nor would really change much long term. I'm incredibly thankful and lucky to have a support system at home to help me through this.
Assuming everything falls into place, the pharmacy is delivering the TPN (IV nutrition) and other medications to my house later this evening, which my step mom will bring to the hospital, connect me to, and then head home. The new home health agency is supposed to come tomorrow to do a dressing change on my PICC (IV line), and make sure that I'm confident in preparing medications. including administering and preparing the Methotrexate injections. I have labs and follow ups with my primary care physician on Monday, and I also need to follow up to see if switching my port is still an option, since ports typically have a lower infection risk than the PICC line (and mine already seems to have some issues with blood return). I have follow ups in San Diego at the end of the month with allergy/immunology and cardiology. The hospital dietician also came by last night to confirm that the current plan is to still get as much of my nutrition as humanly possible by mouth, and also keep me on the TPN, most likely for a couple of months, until my body weight is up. After that, we work on weening off of it, or at least reducing the frequency. The cocktail that constitutes the TPN is regularly adjusted by my doctor and the pharmacist based on my blood tests.
(Warning- paragraph only for those of you interested in the nitty-gritty logistics, otherwise, jump to next paragraph). The Benadryl is the same as it has been before-- I change the bag of medication and tubing that is connected to me daily, and that is attached 24/7, shower, sleeping and all. For Pepcid and the IV steroids, I draw them up into syringes ahead of time, and they have to stay refrigerated-- the Pepcid being twice a day, steroids three times a day (while also titrating the dose down and keeping track of those numbers). The TPN runs for 14/24 hours of the day. Before I can start that, I have to add vitamins and folic acid to the mixture, which ends up being a pretty massive bag. While the TPN is running, I'm carrying the TPN itself, a pump, plus the Benadryl and another pump (which ends up being a solid portion of my entire body weight).
When I initially started the continuous diphenhydramine/Benadryl infusion (CDI) last May, I wrote a lot about a new normal, adjusting to being connected to the pump constantly, and so many new (and scary) considerations. I certainly am feeling that way-- it is pretty overwhelming and scary to have to track and care for everything. I know I'll get through it, just as I did before, but at the moment, I'll let myself go through the anxiety-- and being at HOME will help with that too!
 |
| Part of the "weight gain" care package from my friend Molly (and this wasn't even half!). |
 |
| My cousin Maya drew this page free-handed for me to color! |
(Warning- paragraph only for those of you interested in the nitty-gritty logistics, otherwise, jump to next paragraph). The Benadryl is the same as it has been before-- I change the bag of medication and tubing that is connected to me daily, and that is attached 24/7, shower, sleeping and all. For Pepcid and the IV steroids, I draw them up into syringes ahead of time, and they have to stay refrigerated-- the Pepcid being twice a day, steroids three times a day (while also titrating the dose down and keeping track of those numbers). The TPN runs for 14/24 hours of the day. Before I can start that, I have to add vitamins and folic acid to the mixture, which ends up being a pretty massive bag. While the TPN is running, I'm carrying the TPN itself, a pump, plus the Benadryl and another pump (which ends up being a solid portion of my entire body weight).
 |
| Very excited to ditch this view and the never ending wire tangle. |
When I initially started the continuous diphenhydramine/Benadryl infusion (CDI) last May, I wrote a lot about a new normal, adjusting to being connected to the pump constantly, and so many new (and scary) considerations. I certainly am feeling that way-- it is pretty overwhelming and scary to have to track and care for everything. I know I'll get through it, just as I did before, but at the moment, I'll let myself go through the anxiety-- and being at HOME will help with that too!
Tuesday, August 14, 2018
The Waiting Game
Although I would LOVE to say that I am back at home catching up on sleep, I am stuck in the ever so familiar holding pattern- the waiting game. Since my last post, I was able to tolerate the final day of of IVIG, which we were hoping would provide enough of a boost to see an improvement in my symptoms, and as always, to decrease the ever-so hated steroids. Each round of IVIG doesn't necessarily make a difference independently, which was true in this scenario. High dose IV steroids have now been building up for almost two weeks, which should mean that we able to decrease the dose slowly- yet, again, my body doesn't seem to be a fan of the agenda.
The IV steroids work. But that's also the problem. Although they help reduce my symptoms, reduce the severity and frequency of reactions, there are countless side and secondary effects that make them dangerous long term. I have already developed osteoporosis from them, and long term use increases the risk for metabolic issues, diabetes, advanced bone degeneration, and a whole host of other issues.
To try to make up the "gap" that the IV steroids fill, I have been on multiple immunosuppressants for a few years. Now that we know for a fact that my gut absorption is close to nada, we discontinued two of my immunosuppressants. Instead, we have now added Methotrexate, which is another immunosuppressant and chemotherapy medication. Although its technically a chemo, I am on a low dose, and side effects are supposed to be minimal, and primarily related to mouth sores, hair loss, and issues with blood counts. It is an injection that I will receive once a week.
I have received one dose of the new medication, but unfortunately, even if it is helpful (which we have no guarantee of), it can take 3-4 weeks plus to see a difference. In addition, like the other immunosuppressants I have taken, it is "broad spectrum," meaning that it impacts my entire immune system, but may not be specific enough to address the particular autoimmune process that is happening for me. I'm hoping that over time, as that does builds up, and because it is an injection instead of an oral medication, that it can help with the steroid reduction.
So, for now, we wait. I still feel pretty guilty being a "negative Nelly," but reasonably, I'm frustrated. We're all frustrated. The team here has been amazing, and looking into a variety of treatment options, research, etc. We know what's happening, we know the treatment options, but there just isn't a whole lot of targeted therapies that we can try and apply. It is just going to take time for things to mellow out, and to slowly decrease the steroids. Originally, the game plan was to have me out today or tomorrow, but now it is looking like I would be going home later this week if things go ok. I've burned through quite a few coloring and sticker books to avoid going stir crazy from not leaving the unit in more than a week :P There have been some more canine and human visitors which also helps the time go by :)
On the bright side, having nutrition, vitamins and proper electrolyte levels through the TPN has made a major difference, even though I'm not thrilled about going home on it. I am working on trying to eat as much as I can in addition to the TPN to help keep my gut somewhat functional. My electrolytes are finally starting to stabilize, and I'm not having any more of the weird cardiac episodes. The PICC line in my arm that I am receiving meds through is being finicky, but we are trying to preserve it for as long as possible. I suppose "counting my blessings" is right in this context, that I have the ability to go home with support like TPN so I can avoid living in the hospital. I'm hoping my next post will be one heading home!
Labels:
careaboutrare,
chronic illness,
friendship,
mastcell,
mcad,
spoonie
Friday, August 10, 2018
IVIG Day #2, TPN Day #4
Thanks again for everyone's well wishes and support over the last couple of days! It certainly has felt like a bit of a time warp, which I guess is kind of to be expected when you're in the same room for a while. Since my last post, I had my first three days of Total Parenteral Nutrition (TPN), and two days of IVIG (intravenous immunoglobulin).
For those of you who have been following my story for a while, I have been receiving IVIG monthly, and then bi-weekly since November. My first admission of the past couple of weeks occurred after an adverse reaction to my standard IVIG infusion. IVIG has helped immensely, so we were not ready to give that up unless there was really persuasive evidence that I could no longer tolerate IVIG. To test that, we have been doing 1/3 of my usual IVIG dose each day, with the third and final day tomorrow. With the high dose IV steroids I have been receiving for almost 2 weeks, these infusions went smoother, which overall is a good sign. I still react to the infusions, but have responded well to the meds to treat the reaction symptoms.
The first 24 hours on the TPN was kind of rough. I felt even more run down/beat up than usual, almost as if I had the flu, and some reaction symptoms. My body seems to have adjusted well to it, and now that I'm actually getting the nutrition that I have been so short on for so long, I am already noticing a difference in my strength, energy, and thinking. When I came into the hospital, I could barely walk because I was so weak, and experiencing arrhythmias from low electrolytes, which have now almost entirely resolved.
We are still working my way up to a "full" daily dose of TPN. Because of how malnourished I was, they have to slowly add in nutrition to avoid what is known as Refeeding Syndrome. Refeeding Syndrome occurs when the body is overwhelmed by nutrients if they are introduced too quickly after extended periods of malnutrition, and can cause issues with electrolytes, metabolism, etc. They watch for it closely through daily labs, and adjust the "cocktail" of vitamins, minerals, calories, and electrolytes in the TPN accordingly.
My labs are still showing significant issues with electrolytes, which again, is absolutely no surprise because of the levels I was starting with and the continued auto-immune process impacting my kidneys and gut. In addition to the TPN, I have been getting additional infusions of potassium and phosphorus.
I haven't gained weight (supposed to take time, not overnight), and my electrolytes are improved but certainly not resolved, which means that the plan is to continue TPN after I am discharged. I mentioned this in my last post as well, but usually TPN is used for individuals with little to no ability to consume food or use their GI tract. In my case, it is being used as a supplement to get me closer to a healthy weight, maintain electrolytes, and a minimum of 1,000 calories a day of intake. The hope is that over time, we will wean me off the TPN in a few months. I still have concerns of infection, practicality, and the impact on the rest of my organs related to the TPN, but at this point, it's what we need to sustain me in order to even explore other treatment options down the line.
After the final day of IVIG tomorrow, the plan is to over the weekend to slowly start decreasing the IV steroids. I'm still on a higher dose of steroids than I was re-admitted on, so that also is going to take time and patience. Real conversations of discharge haven't started yet (other than confirming that the TPN is sticking around), so realistically speaking, we are looking at mid next week.
I'm of course still majorly bummed about graduate school and the overall conversations about treatment options and such, but I'm glad we are at the very least seeing progress. My def The team here that is part of the UCLA network has been amazing, compassionate, patient, and realistic about the situation at hand. They have taken the time to listen to us/our concerns, and helped me continue to maintain confidence when I bring about concerns or questions. I am a little irked that nobody was more aggressive about nutritional support up until this point, but there's not much that can be done about it.
In the mean time, the snacking/Netflix/coloring/sticker book/tutoring saga continues. I am SO appreciative of the visitors, messages, gifts, food deliveries, and support over the past few days. It really does help pass the time and keep me occupied. I'm hoping for a very uneventful weekend with the steroid decrease so I can make my jailbreak (a much longer one) next week!
Another reminder that if you haven't already, please donate to the Denim Dash for Rare Diseases! It is a walk/roll/stroll 5K (or however much you can) for rare diseases such as those that obviously dramatically impact my life. You do NOT have to participate in the Dash to help out. DONATE HERE!
For those of you who have been following my story for a while, I have been receiving IVIG monthly, and then bi-weekly since November. My first admission of the past couple of weeks occurred after an adverse reaction to my standard IVIG infusion. IVIG has helped immensely, so we were not ready to give that up unless there was really persuasive evidence that I could no longer tolerate IVIG. To test that, we have been doing 1/3 of my usual IVIG dose each day, with the third and final day tomorrow. With the high dose IV steroids I have been receiving for almost 2 weeks, these infusions went smoother, which overall is a good sign. I still react to the infusions, but have responded well to the meds to treat the reaction symptoms.
 |
| Awesome surprises! |
We are still working my way up to a "full" daily dose of TPN. Because of how malnourished I was, they have to slowly add in nutrition to avoid what is known as Refeeding Syndrome. Refeeding Syndrome occurs when the body is overwhelmed by nutrients if they are introduced too quickly after extended periods of malnutrition, and can cause issues with electrolytes, metabolism, etc. They watch for it closely through daily labs, and adjust the "cocktail" of vitamins, minerals, calories, and electrolytes in the TPN accordingly.
My labs are still showing significant issues with electrolytes, which again, is absolutely no surprise because of the levels I was starting with and the continued auto-immune process impacting my kidneys and gut. In addition to the TPN, I have been getting additional infusions of potassium and phosphorus.
 |
| Yellow= TPN, White= Lipids, Clear = Benadryl |
I haven't gained weight (supposed to take time, not overnight), and my electrolytes are improved but certainly not resolved, which means that the plan is to continue TPN after I am discharged. I mentioned this in my last post as well, but usually TPN is used for individuals with little to no ability to consume food or use their GI tract. In my case, it is being used as a supplement to get me closer to a healthy weight, maintain electrolytes, and a minimum of 1,000 calories a day of intake. The hope is that over time, we will wean me off the TPN in a few months. I still have concerns of infection, practicality, and the impact on the rest of my organs related to the TPN, but at this point, it's what we need to sustain me in order to even explore other treatment options down the line.
After the final day of IVIG tomorrow, the plan is to over the weekend to slowly start decreasing the IV steroids. I'm still on a higher dose of steroids than I was re-admitted on, so that also is going to take time and patience. Real conversations of discharge haven't started yet (other than confirming that the TPN is sticking around), so realistically speaking, we are looking at mid next week.
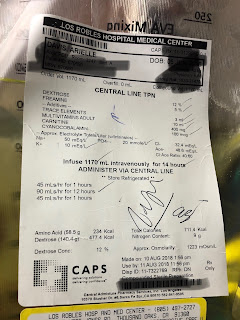 |
| For those of you who are curious what goes into TPN. Lipids are a separate bag. |
In the mean time, the snacking/Netflix/coloring/sticker book/tutoring saga continues. I am SO appreciative of the visitors, messages, gifts, food deliveries, and support over the past few days. It really does help pass the time and keep me occupied. I'm hoping for a very uneventful weekend with the steroid decrease so I can make my jailbreak (a much longer one) next week!
Another reminder that if you haven't already, please donate to the Denim Dash for Rare Diseases! It is a walk/roll/stroll 5K (or however much you can) for rare diseases such as those that obviously dramatically impact my life. You do NOT have to participate in the Dash to help out. DONATE HERE!
Labels:
careaboutrare,
chronic illness,
dysautonomia,
mastcell,
mastcelldisease,
mcad,
spoonie
Tuesday, August 7, 2018
Well, that was fast--Tough Decisions.
Usually I can come up with some clever introduction to my blog posts, but for this one, I'm kind of at a loss. After my last blog post, I was discharged Saturday afternoon with the IV steroids to be able to continue the steroid taper from the comfort of home, and eventually gradually switch to oral/liquid steroids while also trying to get my weight back up to a healthy level.
Yesterday I was going to a follow up appointment with my primary care doctor, and prior to leaving, I started experiencing the same weird feeling in my chest/arrythmia that I have been feeling intermittently. It came and went, but it was enough to make more really dizzy, nauseous, and short of breath. I got to my doctor's office, and at that point, it seemed to fuel some sort of mast cell reaction. They called 911, and I was back off to the hospital.
When I got here, they gave me the usual anaphylaxis protocol, and also took blood work. Those labs indicated what we already knew and had been seeing in my labs for weeks, severe malnourishment and failure to absorb medications and nutrients. They admitted me back to the ICU Stepdown Unit/PCU Unit that I had been on for the latter part of my last admission, and gave me IV electrolytes overnight.
 After speaking with the team here and nutritionists, they decided to start me on TPN, or Total Parenteral Nutrition (LINK). TPN is a cocktail of vitamins, minerals, lipids, fats, etc. that provide complete nutrition via a central line, like the PICC that was placed last week or my port. It takes the GI tract out of the equation in terms of what is getting absorbed, since it bypasses the GI tract entirely, which is why they elected for TPN instead of a nasal or surgical feeding tube. It runs for 12-14 hours a day and provides an entire day's worth of calories and nutrition. While inpatient, they take labs daily, and build a "cocktail" based upon whichever nutritional deficits they are seeing. On an outpatient basis, these labs are usually once a week.
After speaking with the team here and nutritionists, they decided to start me on TPN, or Total Parenteral Nutrition (LINK). TPN is a cocktail of vitamins, minerals, lipids, fats, etc. that provide complete nutrition via a central line, like the PICC that was placed last week or my port. It takes the GI tract out of the equation in terms of what is getting absorbed, since it bypasses the GI tract entirely, which is why they elected for TPN instead of a nasal or surgical feeding tube. It runs for 12-14 hours a day and provides an entire day's worth of calories and nutrition. While inpatient, they take labs daily, and build a "cocktail" based upon whichever nutritional deficits they are seeing. On an outpatient basis, these labs are usually once a week.
 In theory and in the short term, TPN is literally life saving. However, the long term risk profile, risk of complications, and impact on quality of life can be challenging. The current plan is to use TPN for a week + to get my weight up out of the danger zone, and provide a buffer. We suspect that at this point, the autoimmune process that has been ravaging my system is partially fueled by the fact that my body is trying to attack tissues for energy sources. Once we have gotten me out of the danger zone, then we will work on getting me off TPN as soon as humanly possible.
In theory and in the short term, TPN is literally life saving. However, the long term risk profile, risk of complications, and impact on quality of life can be challenging. The current plan is to use TPN for a week + to get my weight up out of the danger zone, and provide a buffer. We suspect that at this point, the autoimmune process that has been ravaging my system is partially fueled by the fact that my body is trying to attack tissues for energy sources. Once we have gotten me out of the danger zone, then we will work on getting me off TPN as soon as humanly possible.
In the mean time, I am supposed to eat as much and as frequently as possible to make sure that my GI tract doesn't take an even more extended hiatus than it already has. I am trying to nibble throughout the day, use supplements like Ensure, etc, again to try to avoid TPN complications and hopefully need it as minimally as possible.
That being said, I was supposed to move into graduate housing at the end of the month to begin my MSW program. In light of recent events, the shift in what our plan going forward is, and the timing of everything, I had to make the extraordinarily difficult decision to defer enrollment in my Master's program for a year.
To be entirely honest, I'm pretty heartbroken. I know grad school will wait for me, and that I need to be focusing on my health, but as I mentioned in my last post, I'm naturally frustrated. I am confident in my team's ability to manage things and to anything and everything necessary to get me back up to speed as soon as possible. I'm also scared of TPN complications, but I know that at this point, I don't have any other choices. While I'm here, we also are going to continue to ween down on the steroids whenever possible while trying to also avoid any more major mast cell episodes.
Once I'm discharged, depending on where we are at with TPN, I"ll either get my port swapped to a double lumen (2 part), or a line called a Hickman, which is similar to the PICC line that they placed in my arm, but in my chest. For TPN, it sometimes is less of an infection risk to use a PICC or Hickman in comparison to a port. My educated guess is that I'll be here at least a few days to a week, but it seems to depend on whether my mast cells cooperate with the agenda. In the mean time, I'm working on snacking, tutoring, coloring, and whatever else is distracting and minimally stressful. b
I also feel the need to apologize for the "Debby Downer" kind of post, but for right now, I think writing everything out is helpful for processing. I hope to have a more positive update soon after they start the TPN overnight.
Yesterday I was going to a follow up appointment with my primary care doctor, and prior to leaving, I started experiencing the same weird feeling in my chest/arrythmia that I have been feeling intermittently. It came and went, but it was enough to make more really dizzy, nauseous, and short of breath. I got to my doctor's office, and at that point, it seemed to fuel some sort of mast cell reaction. They called 911, and I was back off to the hospital.
When I got here, they gave me the usual anaphylaxis protocol, and also took blood work. Those labs indicated what we already knew and had been seeing in my labs for weeks, severe malnourishment and failure to absorb medications and nutrients. They admitted me back to the ICU Stepdown Unit/PCU Unit that I had been on for the latter part of my last admission, and gave me IV electrolytes overnight.
 After speaking with the team here and nutritionists, they decided to start me on TPN, or Total Parenteral Nutrition (LINK). TPN is a cocktail of vitamins, minerals, lipids, fats, etc. that provide complete nutrition via a central line, like the PICC that was placed last week or my port. It takes the GI tract out of the equation in terms of what is getting absorbed, since it bypasses the GI tract entirely, which is why they elected for TPN instead of a nasal or surgical feeding tube. It runs for 12-14 hours a day and provides an entire day's worth of calories and nutrition. While inpatient, they take labs daily, and build a "cocktail" based upon whichever nutritional deficits they are seeing. On an outpatient basis, these labs are usually once a week.
After speaking with the team here and nutritionists, they decided to start me on TPN, or Total Parenteral Nutrition (LINK). TPN is a cocktail of vitamins, minerals, lipids, fats, etc. that provide complete nutrition via a central line, like the PICC that was placed last week or my port. It takes the GI tract out of the equation in terms of what is getting absorbed, since it bypasses the GI tract entirely, which is why they elected for TPN instead of a nasal or surgical feeding tube. It runs for 12-14 hours a day and provides an entire day's worth of calories and nutrition. While inpatient, they take labs daily, and build a "cocktail" based upon whichever nutritional deficits they are seeing. On an outpatient basis, these labs are usually once a week. In theory and in the short term, TPN is literally life saving. However, the long term risk profile, risk of complications, and impact on quality of life can be challenging. The current plan is to use TPN for a week + to get my weight up out of the danger zone, and provide a buffer. We suspect that at this point, the autoimmune process that has been ravaging my system is partially fueled by the fact that my body is trying to attack tissues for energy sources. Once we have gotten me out of the danger zone, then we will work on getting me off TPN as soon as humanly possible.
In theory and in the short term, TPN is literally life saving. However, the long term risk profile, risk of complications, and impact on quality of life can be challenging. The current plan is to use TPN for a week + to get my weight up out of the danger zone, and provide a buffer. We suspect that at this point, the autoimmune process that has been ravaging my system is partially fueled by the fact that my body is trying to attack tissues for energy sources. Once we have gotten me out of the danger zone, then we will work on getting me off TPN as soon as humanly possible.In the mean time, I am supposed to eat as much and as frequently as possible to make sure that my GI tract doesn't take an even more extended hiatus than it already has. I am trying to nibble throughout the day, use supplements like Ensure, etc, again to try to avoid TPN complications and hopefully need it as minimally as possible.
That being said, I was supposed to move into graduate housing at the end of the month to begin my MSW program. In light of recent events, the shift in what our plan going forward is, and the timing of everything, I had to make the extraordinarily difficult decision to defer enrollment in my Master's program for a year.
To be entirely honest, I'm pretty heartbroken. I know grad school will wait for me, and that I need to be focusing on my health, but as I mentioned in my last post, I'm naturally frustrated. I am confident in my team's ability to manage things and to anything and everything necessary to get me back up to speed as soon as possible. I'm also scared of TPN complications, but I know that at this point, I don't have any other choices. While I'm here, we also are going to continue to ween down on the steroids whenever possible while trying to also avoid any more major mast cell episodes.
Once I'm discharged, depending on where we are at with TPN, I"ll either get my port swapped to a double lumen (2 part), or a line called a Hickman, which is similar to the PICC line that they placed in my arm, but in my chest. For TPN, it sometimes is less of an infection risk to use a PICC or Hickman in comparison to a port. My educated guess is that I'll be here at least a few days to a week, but it seems to depend on whether my mast cells cooperate with the agenda. In the mean time, I'm working on snacking, tutoring, coloring, and whatever else is distracting and minimally stressful. b
I also feel the need to apologize for the "Debby Downer" kind of post, but for right now, I think writing everything out is helpful for processing. I hope to have a more positive update soon after they start the TPN overnight.
Friday, August 3, 2018
Puppies do Make Everything Better
Well, maybe not everything, but they certainly are a fun change of pace! I had a really rough morning with some weird cardiac symptoms, but I saw three therapy dogs pass my room and it totally cheered me up (not that human visitors are not awesome too, shout out thanks for the visits). The highlight-- the dog in this picture''s name is Epi, after epinephrine. The volunteer asked if I knew what that was- I responded with, "that's why I'm here!" Too perfect of a coincidence.
A health update from my last post-- I was moved from the ICU to the Progressive Care Unit (PCU/ICU stepdown) Tuesday evening. It's nice to finally have a room with an actual toilet, shower, and slightly more room, etc., especially since this admission has unfortunately been longer than anticipated. It can be a little logistically challenging because when I need emergency medications, I need them then and there, but we seem to have refined it to a system.
Despite the IV steroids, the addition of another oral immunosuppressant, and additional Benadryl, I am still having episodes of angioedema (swelling) around my lips, cheeks, and tongue. Thankfully I have only had one episode since moving out of the ICU that has required an epi pen, but nevertheless, I'm frustrated that it has been more than a week and things still aren't fully resolving.
I guess I should know by now that my body doesn't play by the rules, but its still disappointing. In light of the difficulty getting off IV steroids, continued issues of malabsorption of both food and medication, maximize comfort, and decrease infection risk, the team is ok with sending me home with IV steroids and the intention of gradually lowering those and transitioning to oral steroids, but liquid instead of pills. The IV immune-modulating medication will be added once things are more stable a month or two down the line.
There was one more inpatient dose decrease in steroids this morning. If things go ok this evening and through tomorrow, I should be able to go home tomorrow. The pharmacy has been great (as always) and is supposed to meet me at home with my supplies. We had a hiccup this afternoon with home health nursing. I have not always seen eye to eye with the nursing agency since I moved back home, but today, where they were argumentative, asking for cash pay despite insurance coverage, and overall creating additional unnecessary hurtles. This agency is totally independent of the pharmacy, and the pharmacy has their own nursing in addition to contracted agencies, so it shouldn't be any issue, but nevertheless seems like a pointless speed bump.
Once I get out of here, I'll be able to have a better gage of my plans for the near future. In the very immediate future, the plan is to continue the medications at home, the new oral medication, the new IV medication (Rituxan) down the road, another attempt at IVIG in a week, and getting my (currently de-accessed) single port switched to a double lumen so the PICC can be removed ASAP. Current plan is move into graduate housing the last week of August if things stay stable. My new wheelchair should come in about 2 weeks.
In the mean time, I'm occupying myself with online tutoring and orange is the new black, and surrounded by copious amounts of snacks in the attempt to get my weight back up to normal. I haven't been outside in a week now, so fresh air is going to feel amazing. I'm hoping to be able to binge watch Sacha Baron Cohen's new show over the weekend because I heard some positive reviews :P Plus, the ice cream at home is a lot taster than these damn Ensures!
PS-- If you haven't already, please donate to the Denim Dash for Rare Diseases! It is a walk/roll/stroll 5K (or however much you can) for rare diseases such as those that obviously dramatically impact my life. You do NOT have to participate in the Dash to help out. DONATE HERE!
A health update from my last post-- I was moved from the ICU to the Progressive Care Unit (PCU/ICU stepdown) Tuesday evening. It's nice to finally have a room with an actual toilet, shower, and slightly more room, etc., especially since this admission has unfortunately been longer than anticipated. It can be a little logistically challenging because when I need emergency medications, I need them then and there, but we seem to have refined it to a system.
Despite the IV steroids, the addition of another oral immunosuppressant, and additional Benadryl, I am still having episodes of angioedema (swelling) around my lips, cheeks, and tongue. Thankfully I have only had one episode since moving out of the ICU that has required an epi pen, but nevertheless, I'm frustrated that it has been more than a week and things still aren't fully resolving.
I guess I should know by now that my body doesn't play by the rules, but its still disappointing. In light of the difficulty getting off IV steroids, continued issues of malabsorption of both food and medication, maximize comfort, and decrease infection risk, the team is ok with sending me home with IV steroids and the intention of gradually lowering those and transitioning to oral steroids, but liquid instead of pills. The IV immune-modulating medication will be added once things are more stable a month or two down the line.
There was one more inpatient dose decrease in steroids this morning. If things go ok this evening and through tomorrow, I should be able to go home tomorrow. The pharmacy has been great (as always) and is supposed to meet me at home with my supplies. We had a hiccup this afternoon with home health nursing. I have not always seen eye to eye with the nursing agency since I moved back home, but today, where they were argumentative, asking for cash pay despite insurance coverage, and overall creating additional unnecessary hurtles. This agency is totally independent of the pharmacy, and the pharmacy has their own nursing in addition to contracted agencies, so it shouldn't be any issue, but nevertheless seems like a pointless speed bump.
Once I get out of here, I'll be able to have a better gage of my plans for the near future. In the very immediate future, the plan is to continue the medications at home, the new oral medication, the new IV medication (Rituxan) down the road, another attempt at IVIG in a week, and getting my (currently de-accessed) single port switched to a double lumen so the PICC can be removed ASAP. Current plan is move into graduate housing the last week of August if things stay stable. My new wheelchair should come in about 2 weeks.
In the mean time, I'm occupying myself with online tutoring and orange is the new black, and surrounded by copious amounts of snacks in the attempt to get my weight back up to normal. I haven't been outside in a week now, so fresh air is going to feel amazing. I'm hoping to be able to binge watch Sacha Baron Cohen's new show over the weekend because I heard some positive reviews :P Plus, the ice cream at home is a lot taster than these damn Ensures!
PS-- If you haven't already, please donate to the Denim Dash for Rare Diseases! It is a walk/roll/stroll 5K (or however much you can) for rare diseases such as those that obviously dramatically impact my life. You do NOT have to participate in the Dash to help out. DONATE HERE!
Labels:
careaboutrare,
chronic illness,
crowdfunding,
dysautonomia,
friendship,
mastcell,
mastcelldisease,
mcad,
rarediseaseday,
spoonie
Subscribe to:
Posts (Atom)
